If you have recently been diagnosed with Polycystic Ovary Syndrome (PCOS), your first instinct was probably to hit Google. And if you did, you likely walked away feeling terrified, confused, and convinced that you can never look at a piece of bread again.
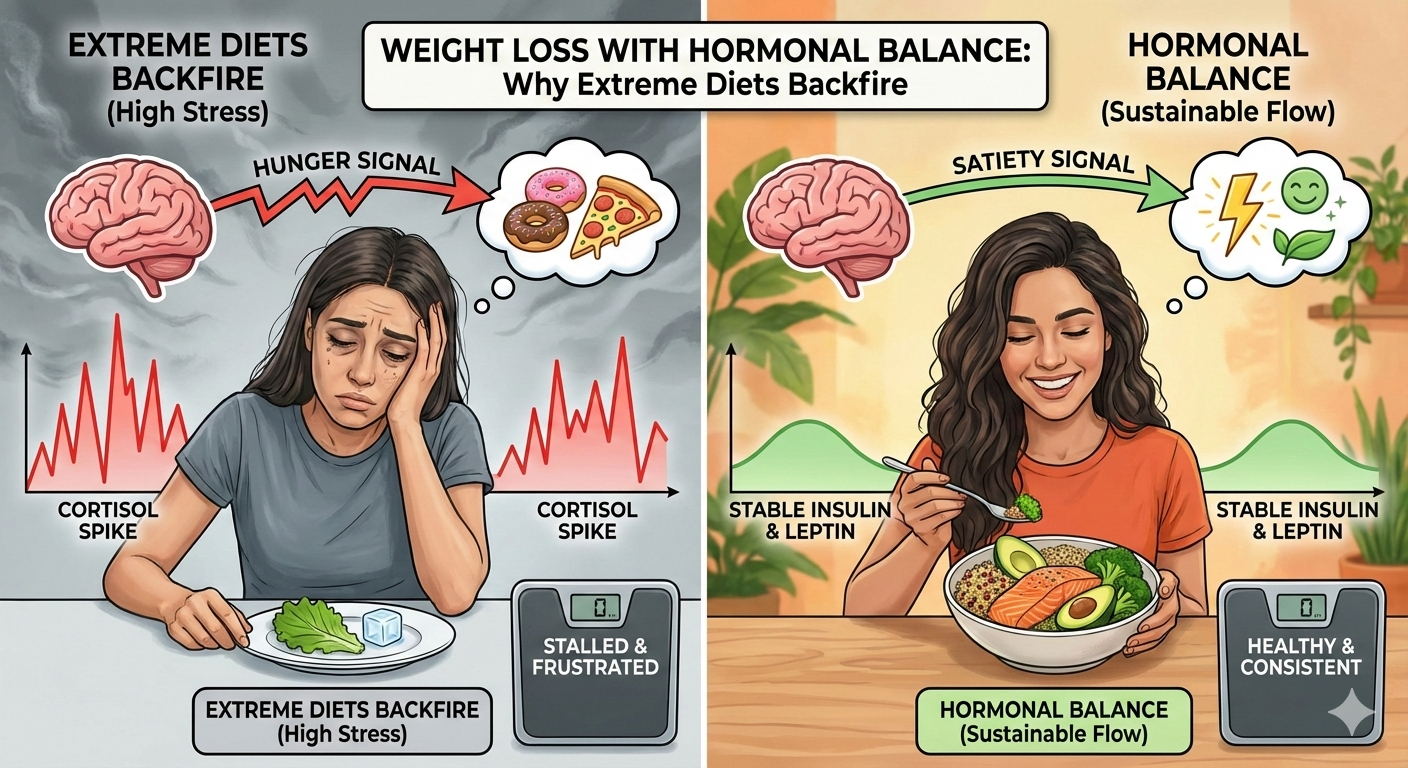
The internet is flooded with “PCOS influencers” promoting restrictive, one-size-fits-all diets. Cut gluten! Cut dairy! Keto or bust! It’s enough to make anyone’s cortisol spike—which, ironically, is the last thing you need.
As a doctor, I’m here to tell you that managing PCOS doesn’t require you to be miserable. In fact, sustainable management is often about adding nutrition rather than ruthlessly subtracting it. Let’s look at the science, debunk the biggest myths, and focus on what actually moves the needle for your hormones.
👉Understanding PCOD: Rising Trends, Health Implications, and Ayurvedic Remedies for Balance
Myth #1: “You Must Cut ALL Carbs to Manage PCOS”
This is arguably the most pervasive myth out there. The logic seems sound on the surface: PCOS is often driven by insulin resistance (where your cells don’t respond well to insulin, leading to high blood sugar). Since carbohydrates spike insulin, cutting them out entirely should fix the problem, right?
The Doctor’s Explanation: While it is true that refined carbohydrates (sugar, white flour, pastries) can worsen insulin resistance, your body—and your hormones—actually need carbohydrates for energy and thyroid function. Going “zero carb” can increase stress hormones, which may actually stall ovulation.
The goal isn’t no carb; it’s slow carb.
We want to focus on the Glycemic Index (GI). Low-GI carbohydrates break down slowly, preventing that massive insulin spike. Think quinoa, oats, sweet potatoes, and berries.
The Science: A meta-analysis of multiple studies confirmed that while lower-carbohydrate diets can improve insulin sensitivity, the “quality” of the diet matters immensely. You do not need to be in ketosis to see results; you simply need to stabilize your blood sugar curve.
Myth #2: “Every Woman with PCOS Needs to be Gluten-Free and Dairy-Free“
If I had a nickel for every time a patient asked if they needed to throw out their yogurt, I could fund a research lab. The narrative is that gluten and dairy are inherently “inflammatory” and will cause cysts to grow.
The Doctor’s Explanation: Let’s look at the nuance. Chronic inflammation is a key driver of PCOS. However, unless you have Celiac disease, a non-celiac gluten sensitivity, or a lactose intolerance, there is no strong clinical evidence suggesting that everyone with PCOS needs to eliminate these food groups.
For some women, full-fat dairy (like Greek yogurt) is actually beneficial because it contains calcium, Vitamin D, and probiotics that support gut health. In fact, some research suggests that the fermentation in yogurt can help with the gut microbiome, which plays a massive role in hormone regulation.
That said, if you feel bloated, lethargic, or foggy after eating bread or milk, an elimination diet for 4–6 weeks is a valid experiment. But please, do not blindly cut out food groups just because social media told you to.
The Science: Recent systematic reviews on lifestyle interventions for PCOS emphasize “dietary quality” (like the Mediterranean diet) over specific exclusions. There is currently no scientific consensus that gluten exerts a specific negative effect on PCOS pathology in women without existing sensitivities.
Myth #3: “If You Don’t Lose Weight, Your Symptoms Won’t Improve”
This is the most damaging myth of all. Many doctors unfortunately tell patients, “Just lose weight and your period will come back.” This is gaslighting.
The Doctor’s Explanation: Weight gain in PCOS is often a symptom of the metabolic dysfunction, not just the cause. Telling a woman with high insulin levels to “just eat less” is biologically difficult because her body is in fat-storage mode.
Furthermore, “Lean PCOS” exists. Thin women can still have insulin resistance, missing periods, and high androgens (testosterone). Focusing solely on the scale misses the point. We need to focus on metabolic health—lowering inflammation and insulin—regardless of your weight. When you heal the metabolism, the weight often regulates itself as a side effect.
The Science: Research indicates that lifestyle modifications focusing on metabolic markers (like insulin and androgens) are effective even without massive weight loss. A comprehensive review on dairy and PCOS also highlighted that nutrient-induced inflammation is the culprit, suggesting that what we eat (anti-inflammatory foods) matters more than just caloric restriction.
So, What Actually Works?
Now that we’ve cleared the air, what should you actually put on your plate? Here is a simple, evidence-based “prescription” for your grocery list.
1. The “Clothing” Method for Carbs
Never eat a carbohydrate “naked.” If you are having an apple, pair it with walnuts. If you are having rice, pair it with chicken and avocado. Adding protein, fat, and fiber to a carbohydrate slows down gastric emptying and blunts the insulin spike.
2. Prioritize Anti-Inflammatory Foods
PCOS is a state of low-grade chronic inflammation. Fight fire with food.
-
Omega-3s: Salmon, chia seeds, flaxseeds.
-
Antioxidants: Berries, leafy greens, green tea.
-
Spices: Turmeric and ginger.
3. Consider Inositol
While supplements aren’t a diet, Myo-inositol is one of the most researched compounds for PCOS. It acts as an “insulin sensitizer,” helping your cells open the door to insulin.
4. Eat a Big Breakfast
Research suggests that women with PCOS who eat the majority of their calories in the morning (vs. the evening) see significant drops in insulin and testosterone. A high-protein breakfast (30g of protein) sets your blood sugar stability for the rest of the day.
👉Inositol and PCOS: A Natural Approach to Hormonal Balance
👉The Insulin Resistance Trap in PCOS: How to Break Free Naturally
The Bottom Line
Your PCOS diet shouldn’t feel like a punishment. It should feel like nourishment.
Scientific evidence supports a diet that stabilizes insulin and lowers inflammation—usually a Mediterranean-style approach rich in whole foods, healthy fats, and fiber. You do not need to fear fruit, and you don’t need to fear gluten unless your body specifically rejects it.
Start with small changes. Add protein to your breakfast. Go for a 10-minute walk after meals. Listen to your body, not the noise.
Disclaimer: This post is for educational purposes only and does not constitute medical advice. Always consult with your healthcare provider before making drastic changes to your diet or supplement routine.

Akanksha Sharma
Dr. Akanksha Sharma (MD), Head Writer and creator of AtoZ of Pregnancy, is dedicated to empowering women, parents, and families through 360-degree knowledge. She and her team provide evidence-based advice to guide families through pregnancy, parenting and beyond.





Leave a Reply