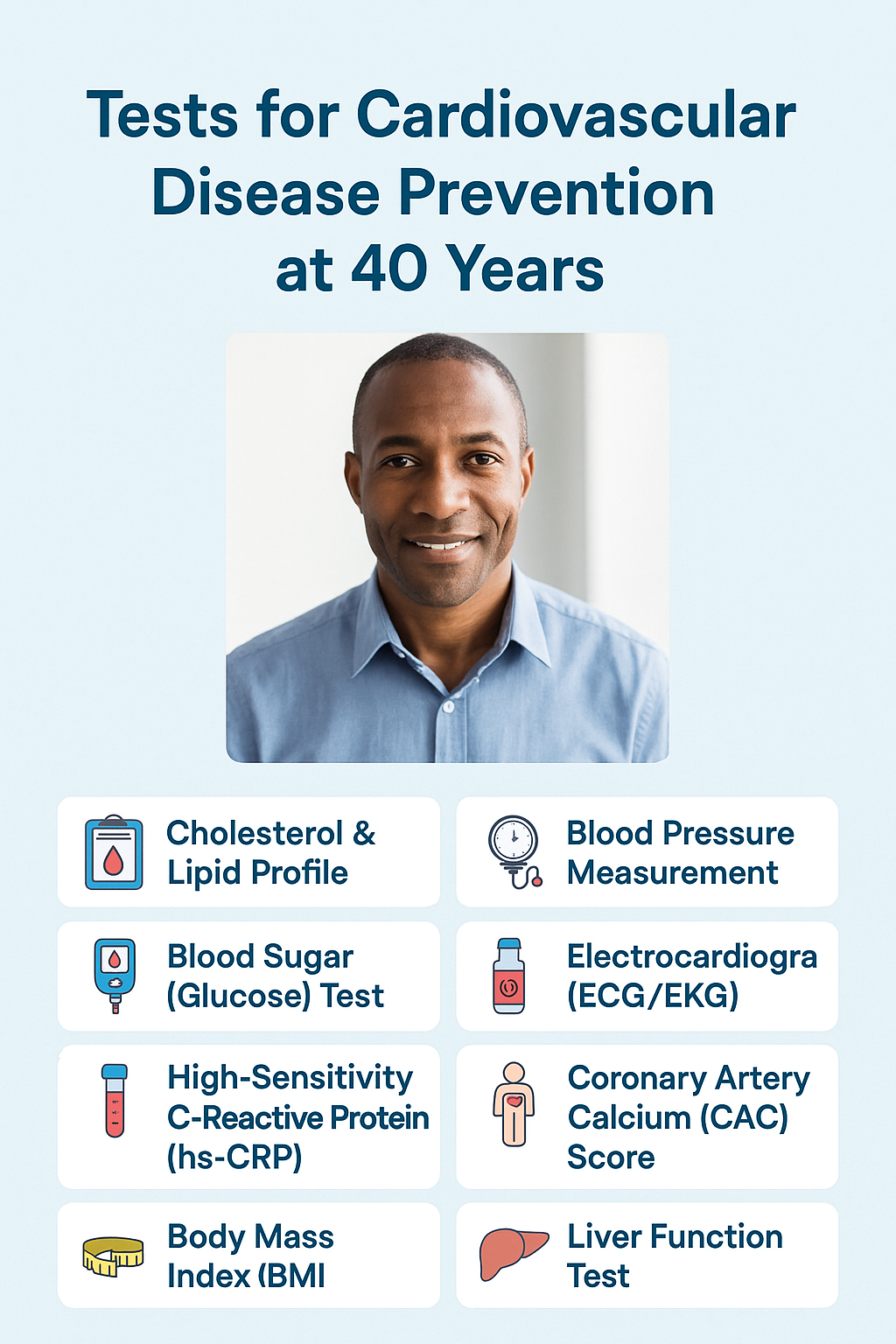
As we hit the milestone of 40, it becomes even more important to take control of our health and prioritize cardiovascular disease (CVD) prevention. CVD is one of the leading causes of death globally, but with early detection and the right lifestyle changes, we can reduce our risks significantly.
In this blog post, we’ll look at the key tests recommended for people aged 40 and above to assess their heart health and prevent future complications.
1. Cholesterol and Lipid Profile 🧪
A comprehensive lipid profile is one of the most crucial tests to determine your cholesterol levels. The test measures:
-
Total cholesterol
-
LDL (Low-Density Lipoprotein) – often called “bad cholesterol”
-
HDL (High-Density Lipoprotein) – known as “good cholesterol”
-
Triglycerides – another type of fat found in the blood
Why is it important?
High levels of LDL cholesterol and triglycerides increase the risk of plaque buildup in your arteries, which can lead to heart disease. HDL cholesterol helps remove excess cholesterol from the bloodstream, so it’s important to keep those levels high.
When Should You Get a Lipid Profile?
-
For healthy adults:
-
A lipid profile is typically recommended every 4–6 years for adults aged 20 and older.
-
After age 40, it’s generally recommended to have one done at least every 1–2 years to monitor cardiovascular risk.
-
-
For those with risk factors:
-
If you have risk factors such as a family history of heart disease, smoking, diabetes, high blood pressure, or obesity, you may need a lipid profile more frequently, often annually.
-
-
For those with existing cardiovascular disease or high cholesterol:
-
If you already have heart disease or high cholesterol, your doctor may recommend more frequent testing, such as every 3–6 months, to monitor treatment effectiveness.
-
How to Prepare for a Lipid Profile
-
Fasting: In most cases, you’ll need to fast for 9–12 hours before a lipid profile test, as food intake can temporarily alter lipid levels, especially triglycerides.
-
Hydration: Drink plenty of water before the test, but avoid eating or drinking anything with calories.
-
Medication and lifestyle factors: Let your doctor know about any medications you’re taking or recent lifestyle changes, as these can affect the results.
2. Blood Pressure Measurement 💉
High blood pressure (hypertension) can damage your arteries and increase your risk of heart disease. A simple blood pressure test will give you two key readings: systolic (pressure during heartbeats) and diastolic (pressure between beats).
Why is it important?
Blood pressure consistently higher than 140/90 mmHg increases your risk of heart failure, stroke, and kidney disease.
When to test?
-
Frequency: At least once every two years if normal (less than 120/80 mmHg), but more frequently if elevated.
3. Blood Sugar (Glucose) Test 🩸
Diabetes is a major risk factor for CVD. High blood sugar levels over time can damage your heart, blood vessels, and kidneys.
Why is it important?
Testing for diabetes helps identify whether you have high blood sugar or are at risk for developing diabetes, which is critical in preventing CVD.
When to test?
-
Frequency: Every 3 years starting at age 45, or earlier if you have risk factors like obesity, family history, or high blood pressure.
4. Electrocardiogram (ECG/EKG) 🫀
An ECG measures the electrical activity of your heart. It can identify irregular heart rhythms (arrhythmias), signs of a past heart attack, and other heart-related issues.
Why is it important?
It helps detect heart problems early, even before symptoms appear. It’s especially important if you experience symptoms like chest pain, dizziness, or shortness of breath.
When to test?
-
Frequency: If you have symptoms or a family history of heart disease, an ECG is recommended.
5. High-Sensitivity C-Reactive Protein (hs-CRP) Test ⚡
This blood test measures inflammation levels in the body. Inflammation is a major contributor to atherosclerosis (hardening of the arteries), which can lead to heart attacks and strokes.
Why is it important?
Even if you have normal cholesterol levels, inflammation can still contribute to plaque buildup in your arteries, which increases your risk for heart disease. Research suggests that a high hs-CRP/HDL-C ratio is a significant risk factor for CVD, new stroke, and heart problems.
What Do hs-CRP Levels Mean?
The levels of hs-CRP are measured in milligrams per liter (mg/L). The interpretation of the results depends on the following categories:
-
Low Risk (hs-CRP < 1 mg/L)
-
Indicates low levels of inflammation and a lower risk of cardiovascular disease.
-
-
Average Risk (hs-CRP 1–3 mg/L)
-
Suggests moderate levels of inflammation. This may be due to lifestyle factors or existing conditions like obesity or hypertension.
-
-
High Risk (hs-CRP > 3 mg/L)
-
Indicates high levels of inflammation, which may increase the risk of heart disease and other chronic health conditions. It is important to investigate further if this level is found, especially in people with other cardiovascular risk factors.
-
When is hs-CRP tested?
-
Heart disease risk assessment: It is often used alongside other tests (such as cholesterol levels) to assess the risk of heart disease, particularly in people who may not have any obvious symptoms but have other risk factors (like high cholesterol, smoking, or a family history of heart disease).
-
Chronic inflammatory conditions: If a person has a known inflammatory condition (like rheumatoid arthritis or lupus), hs-CRP may be used to monitor disease activity and assess response to treatment.
-
Obesity, metabolic syndrome, and diabetes management: hs-CRP is also used in managing conditions like obesity and type 2 diabetes, as inflammation plays a role in their development and progression.
Frequency of Testing:
-
Heart health risk: If you’re at moderate risk for heart disease or have risk factors (like high blood pressure, high cholesterol, or a family history of heart disease), it may be done every 1-2 years as part of a comprehensive cardiovascular risk assessment.
-
Chronic inflammatory diseases: If you have conditions like rheumatoid arthritis or inflammatory bowel disease, hs-CRP levels may be checked more frequently to monitor disease activity and inflammation levels.
6. Coronary Artery Calcium (CAC) Score 🦠
A CAC scan uses a CT scan to detect calcium buildup in the coronary arteries, which is an early sign of atherosclerosis.
Why is it important?
If you have a family history of heart disease or multiple risk factors but no obvious symptoms, a CAC score test can help gauge your risk of future heart disease.
When to test?
-
If you have no symptoms or risk factors:
-
One-time screening: For individuals with no known heart disease risk factors and no symptoms, a single CAC scan may be done to assess baseline heart health, particularly for those with a moderate risk of developing cardiovascular disease.
-
Re-screening: If your initial score is low (i.e., no detectable calcium), there may be no need for a follow-up for at least 5–10 years, depending on your risk profile.
2. If you have risk factors (e.g., family history of heart disease, high cholesterol, hypertension, diabetes, smoking):
-
Every 3–5 years: Individuals with a moderate to high risk of cardiovascular disease may consider periodic scans, depending on other risk factors and initial CAC score results. The frequency can vary based on individual risk factors and the advice of a healthcare provider.
3. If you have symptoms or a known history of heart disease:
-
As recommended by your doctor: In cases where a person has existing cardiovascular conditions or symptoms, the CAC test may be repeated more frequently, as advised by a healthcare professional.
Important Notes:
-
The CAC score is not always necessary for everyone over 40, especially if other risk factors are already well-managed or assessed by other tests (e.g., cholesterol levels, blood pressure).
-
It’s always best to consult with a healthcare provider to determine whether a CAC test is needed and how often it should be repeated based on your personal health profile.
-
7. Body Mass Index (BMI) Measurement 📏
BMI is a simple measure that helps identify whether you are overweight, underweight, or at a healthy weight.
Why is it important?
Being overweight or obese significantly increases the risk of developing heart disease, diabetes, and high blood pressure. Research suggests that obesity is associated with shorter longevity and significantly increased risk of cardiovascular morbidity and mortality compared with normal BMI.
When to test?
-
Frequency: Annually, or more frequently if you are trying to lose or gain weight.
8. Liver Function Test 🧑⚕️
Liver disease can contribute to high cholesterol and hypertension, which in turn increase the risk for heart disease.
Why is it important?
A healthy liver helps regulate fat and sugar levels in the body. Monitoring liver function is especially important for those with obesity or high cholesterol. Evidence suggests that a doubling of GGT is associated with a 34% increase in the risk of incident cardiovascular events.
When to test?
-
For Healthy Adults with No Risk Factors:
-
Frequency: Typically, an LFT is done as part of a routine health checkup once every 1-2 years.
-
If you’re otherwise healthy with no symptoms or known liver risk factors (such as alcohol use, obesity, or family history of liver disease), this frequency is usually sufficient.
-
-
For Individuals with Risk Factors (e.g., Obesity, Alcohol Consumption, Family History of Liver Disease):
-
Frequency: LFTs may be recommended more often, generally annually or every 6-12 months.
-
If you are overweight, consume alcohol, or have conditions like diabetes, this will help monitor any potential liver damage.
-
-
For Individuals with Existing Liver Conditions (e.g., Hepatitis, Fatty Liver Disease, Cirrhosis):
-
Frequency: If you have a diagnosed liver disease, your doctor may recommend more frequent monitoring, such as every 3-6 months, to track the progression of the condition and guide treatment.
-
In cases of advanced liver disease, LFTs might be monitored even more frequently based on your healthcare provider’s assessment.
-
-
If You’re Taking Medications That Affect the Liver:
-
Frequency: If you’re on medications known to impact liver function (e.g., statins, certain pain relievers, or chemotherapy), your doctor may monitor your LFTs more regularly, such as every 3-6 months.
-
Special Considerations:
-
Symptoms or New Health Concerns: If you develop symptoms like unexplained fatigue, jaundice (yellowing of the skin or eyes), abdominal pain, or swelling, LFTs should be done immediately to rule out liver issues.
-
Post-Procedure Monitoring: After certain procedures, such as liver biopsies or surgeries, LFTs may be monitored more frequently to ensure proper recovery.
-
Frequency: Annually, or if you have a history of liver problems, excessive alcohol use, or are on medications that affect the liver then more frequently.
Conclusion 🏥
Cardiovascular disease doesn’t happen overnight, and many of its early signs can be detected with simple tests. Starting at age 40, it’s essential to stay proactive about heart health. Regular screenings, alongside a healthy lifestyle that includes a balanced diet, exercise, and stress management, can help you maintain good heart health for years to come.
Stay informed, stay healthy, and make your heart a priority! ❤️
👩⚕️ Need a Personalized Cardiovascular Reset Diet Plan?
We offer a 15-Day CVD Reset with:
-
Nutritional protocols
-
Physical activity guidance
-
Anti-inflammatory meals
-
WhatsApp tracking support
👉Click here to start your journey today!
References:
- Alloubani A, Nimer R, Samara R. Relationship between Hyperlipidemia, Cardiovascular Disease and Stroke: A Systematic Review. Curr Cardiol Rev. 2021;17(6):e051121189015.
- Messerli FH, Williams B, Ritz E. Essential hypertension. Lancet. 2007 Aug 18;370(9587):591-603.
- Nanayakkara N, Curtis AJ, Heritier S, Gadowski AM, Pavkov ME, Kenealy T, Owens DR, Thomas RL, Song S, Wong J, Chan JC, Luk AO, Penno G, Ji L, Mohan V, Amutha A, Romero-Aroca P, Gasevic D, Magliano DJ, Teede HJ, Chalmers J, Zoungas S. Impact of age at type 2 diabetes mellitus diagnosis on mortality and vascular complications: systematic review and meta-analyses. Diabetologia. 2021 Feb;64(2):275-287.
- Gao Y, Wang M, Wang R, Jiang J, Hu Y, Wang W, Wang Y, Li H. The predictive value of the hs-CRP/HDL-C ratio, an inflammation-lipid composite marker, for cardiovascular disease in middle-aged and elderly people: evidence from a large national cohort study. Lipids Health Dis. 2024 Mar 1;23(1):66.
- Khan SS, Ning H, Wilkins JT, Allen N, Carnethon M, Berry JD, Sweis RN, Lloyd-Jones DM. Association of Body Mass Index With Lifetime Risk of Cardiovascular Disease and Compression of Morbidity. JAMA Cardiol. 2018 Apr 1;3(4):280-287.
- Yilmaz Y. Liver function tests: Association with cardiovascular outcomes. World J Hepatol. 2010 Apr 27;2(4):143-5.

Akanksha Sharma
Dr. Akanksha Sharma, Head Writer and creator of AtoZ of Pregnancy, is dedicated to empowering women, parents, and families through 360-degree knowledge. She and her team provide evidence-based advice to guide families through pregnancy, parenting and beyond.