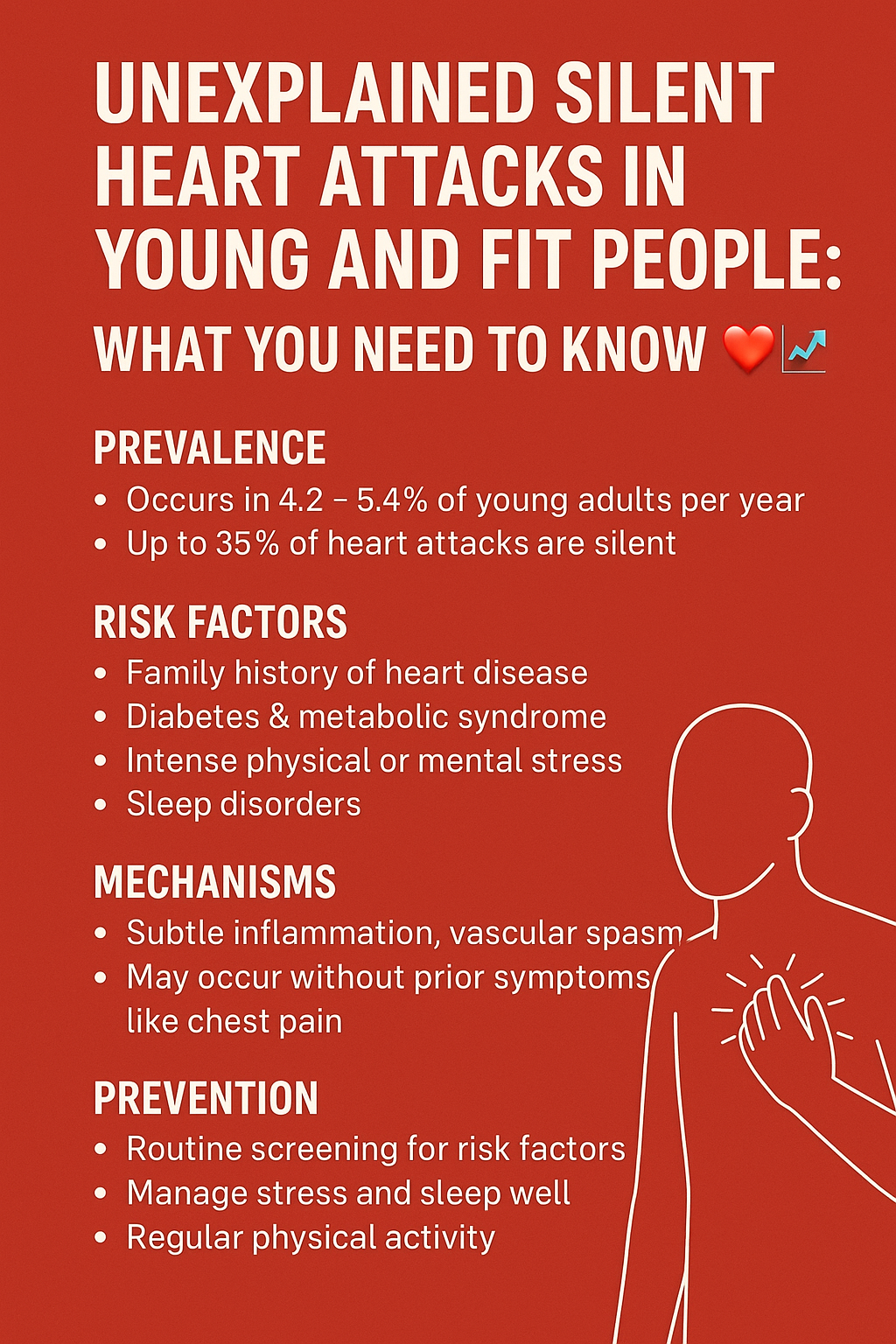
When we think of heart attacks, we often picture older adults with clear risk factors like obesity, smoking, or a sedentary lifestyle. However, emerging data shows a troubling trend: silent or mild heart attacks occurring in young, physically active individuals with no obvious health issues.
These heart attacks often go undiagnosed, yet they pose significant long-term risks to heart health. In this blog, we break down what silent heart attacks are, why they’re happening in the young and fit, and what you can do to prevent them.
❗ What Is a Silent Heart Attack?
A silent heart attack, or silent myocardial infarction (SMI), occurs with minimal or no symptoms. It may be mistaken for indigestion, fatigue, or mild discomfort and often goes undiagnosed until an ECG or imaging test reveals scarring on the heart.
🔹 According to the American Heart Association and Harvard Medical School, 45% of heart attacks are silent.
🤔 Why Are Young and Fit People Affected?
While traditional risk factors are well-known, these lesser-known causes are coming to light:
1. Genetic and Familial Risk
- Lipoprotein(a) [Lp(a)] elevation, familial hypercholesterolemia.
- These genetic issues may not show up in basic lipid profiles.
2. High Stress and Cortisol
- Chronic psychological stress, especially in high-performance individuals, elevates cortisol, which can damage blood vessels and promote plaque formation.
- Apart from directly destroying the endothelium of blood vessels and leading to plaque formation, chronic stress can lead to hyperlipidemia.
3. Overtraining or Under-Recovery
- Intense physical training without proper recovery can lead to inflammation and elevated cardiac biomarkers like troponin.
- “Athlete’s heart” adaptations can sometimes mask cardiac pathology.
4. Post COVID Sequelae
COVID-19 may have triggered a silent wave of heart damage, potentially setting the stage for an unseen pandemic of heart attacks in otherwise young and healthy individuals.
- Cardiac injury was reported in 19% to 28% of COVID-19 patients in Wuhan, China, and was found to be associated with worse patient outcomes
- Patients with COVID-19 have a 16 times increased risk of myocarditis compared without COVID-19.
- Another concern was the COVID-19 vaccine. However, the incidence of myocarditis associated with COVID-19 infection is 100 times higher than the mRNA vaccination
- A study on a group of recently recovered COVID-19 patients in Germany found that 78% showed signs of heart involvement, and 60% still had ongoing heart inflammation, as seen on heart scans. This highlights the need to keep studying how COVID-19 might affect heart health in the long run.
5. Subclinical Atherosclerosis
- Young adults can develop non-calcified plaques, which are more prone to rupture than calcified ones.
- Coronary calcium scans may miss these, but cardiac CT angiography can reveal them.
6. Use of certain Supplements or Energy Drinks
- Stimulants like synephrine, excess caffeine, anabolic steroids can cause vasospasm and sudden cardiac events.
7. Insulin Resistance and Inflammation
- Even fit individuals with high visceral fat, PCOS, or metabolic inflammation may have hidden risk.
🔎How to Detect Silent Cardiac Risk
-
Advanced Lipid Profile
-
Tests to include:
-
ApoB (the most accurate marker of atherogenic particles)
-
Lp(a) (genetic risk marker)
-
Small dense LDL
-
HDL subfractions
-
hs-CRP (for inflammation)
-
-
-
Coronary Artery Calcium (CAC) Score
-
Best for middle-aged and older adults, especially with intermediate risk.
-
Helps determine the need for statins even in low-symptom patients.
-
-
CT Coronary Angiography (CTCA)
-
Detects non-calcified (soft, rupture-prone) plaques.
-
Useful even if CAC = 0, especially in younger or symptomatic patients.
-
-
Echocardiogram
-
Evaluates heart function, chamber size, wall motion abnormalities, and valvular issues.
-
-
Cardiac MRI
-
Gold standard for detecting myocardial inflammation, fibrosis, and scarring
-
Useful post-COVID or for myocarditis evaluation.
-
-
Resting ECG + Exercise Stress Test
-
Can detect arrhythmias, ischemic changes
-
Especially useful if symptoms like palpitations or chest tightness are present
-
-
High-Sensitivity Troponin
-
Detects subclinical myocardial injury
-
Should be combined with other tests in symptomatic individuals
-
-
Genetic Testing (where indicated)
-
For familial hypercholesterolemia, high Lp(a), or early cardiac events in the family
-
Panel testing may include PCSK9, APOE, LDLR, etc.
-
-
Insulin Resistance & Metabolic Markers
-
Fasting insulin, HOMA-IR, and HbA1c
-
Even lean individuals with insulin resistance are at higher CV risk
-
-
Ambulatory Blood Pressure or Holter Monitoring
-
Detects masked hypertension, nocturnal dips, or silent arrhythmias
🧠 Optional Additions for Precision Medicine Settings:
-
Endothelial function testing (e.g., EndoPAT)
-
Arterial stiffness markers (Pulse Wave Velocity)
-
Oxidized LDL or myeloperoxidase (MPO) testing for advanced risk stratification
⚡ What Can Be Done to Prevent Silent Heart Attacks?
🌿 Lifestyle Interventions
- Manage stress through meditation, yoga, and mindfulness.
- Avoid extreme exercise without adequate recovery.
- Get 7–9 hours of quality sleep.
- Stay hydrated and avoid stimulants like excessive caffeine or energy drinks.
🌽 Nutrition for the Heart: Heal with Every Bite
What you eat directly shapes the health of your blood vessels, the strength of your heart muscle, and the level of inflammation in your body. A heart-supportive diet isn’t just about avoiding junk — it’s about actively choosing foods and supplements that reduce inflammation, stabilise cholesterol, and boost vascular function.
🥦 1. Follow an Anti-Inflammatory Diet
Chronic low-grade inflammation is a silent driver of atherosclerosis (plaque buildup) and heart disease. Build your plate with foods that fight inflammation and oxidative stress:
✅ Include:
-
Omega-3-rich foods:
-
Fatty fish (salmon, sardines), walnuts, chia seeds, flaxseeds – help reduce triglycerides and blood pressure.
-
-
Leafy greens:
-
Spinach, kale, moringa – high in potassium, folate, and antioxidants like lutein.
-
-
Colourful vegetables and berries:
-
Rich in polyphenols that support arterial flexibility and reduce oxidative damage.
-
-
Spices like turmeric and ginger:
-
Turmeric’s curcumin is a natural anti-inflammatory and supports endothelial function.
-
-
Whole grains:
-
Oats, barley, quinoa – rich in fibre and beta-glucans that help lower LDL.
-
🚫 2. Cut Out Heart Saboteurs
-
Ultra-processed foods:
-
High in sodium, trans fats, sugar, and additives – all of which increase inflammation and arterial stiffness.
-
-
Trans fats & refined oils:
-
Found in bakery goods, margarine, fried foods. They raise bad cholesterol and reduce good cholesterol.
-
-
High-sugar beverages & snacks:
-
Linked to insulin resistance, obesity, and inflammation.
-
💊 3. Supplements That Support Heart Health
These supplements can enhance cardiovascular resilience, especially when diet alone isn’t enough:
| Supplement | Benefits |
|---|---|
| Omega-3 (Fish Oil) | Reduces triglycerides, inflammation, and supports rhythm stability |
| Magnesium (Citrate/Glycinate) | Helps in BP regulation, heart rhythm, and stress modulation |
| Coenzyme Q10 (CoQ10) | Boosts mitochondrial energy in heart cells, crucial for those on statins |
| Arjuna (Terminalia arjuna) | Ayurvedic herb that improves cardiac output, lowers BP, and supports heart muscle |
| Ashwagandha | Lowers stress-related cortisol, stabilizes BP, and supports nervous system tone |
| Aged Garlic Extract | Improves blood vessel elasticity and reduces arterial plaque |
| L-Citrulline / L-Arginine | Enhances nitric oxide production → vasodilation & better circulation |
| Berberine | Regulates blood sugar & improves lipid profiles (great for metabolic syndrome) |
🧂 4. Balance Your Electrolytes
-
Ensure adequate potassium, magnesium, and calcium through diet or supplementation, especially in hypertensive individuals.
-
Include coconut water, banana, sweet potato, and seeds.
🧘♂️ 5. Mind-Body Nutrition Matters
-
How you eat matters too — eat slowly, chew well, and avoid multitasking during meals.
-
Practice gratitude before meals to engage the parasympathetic (rest-and-digest) state.
🌟 Pro Tip:
Start your day with warm water + lemon + ½ tsp ghee + pinch of turmeric — it soothes the gut, supports bile flow, and sets an anti-inflammatory tone for the day.
⚖️ Medical Monitoring
- Annual ECG and lipid profile (including Lp(a), ApoB)
- Advanced imaging if a strong family history or any exertional symptoms
- Manage even borderline hypertension or insulin resistance
Conclusion: Knowledge Is Protection ✨
Young, healthy people are not immune to heart disease — especially silent attacks. Genetics, stress, inflammation, and undiagnosed issues like Lp(a) or post-viral myocarditis can be silent saboteurs. Being proactive with testing, lifestyle upgrades, and awareness can save lives.
If you’re young and fit but feel “off,” trust your instinct. Get tested. Your heart may be trying to whisper before it screams.
Disclaimer: This blog is for educational purposes only. Consult your physician before starting any new supplement, especially if you have existing health conditions or are taking medications.
🔗 You May Also Find These Readings Helpful:
-
[Essential Tests for Cardiovascular Disease (CVD) Prevention at 40]
-
[6 Top Supplements for Heart Attacks Prevention in Men Over 40]
📚 References
- Vinci P, Di Girolamo FG, Panizon E, Tosoni LM, Cerrato C, Pellicori F, Altamura N, Pirulli A, Zaccari M, Biasinutto C, Roni C, Fiotti N, Schincariol P, Mangogna A, Biolo G. Lipoprotein(a) as a Risk Factor for Cardiovascular Diseases: Pathophysiology and Treatment Perspectives. Int J Environ Res Public Health. 2023 Sep 6;20(18):6721.
- Yao BC, Meng LB, Hao ML, Zhang YM, Gong T, Guo ZG. Chronic stress: a critical risk factor for atherosclerosis. J Int Med Res. 2019 Apr;47(4):1429-1440.
- Baker P, Leckie T, Harrington D, Richardson A. Exercise-induced cardiac troponin elevation: An update on the evidence, mechanism and implications. Int J Cardiol Heart Vasc. 2019 Mar 14;22:181-186.
- Shi S, Qin M, Shen B, Cai Y, Liu T, Yang F, Gong W, Liu X, Liang J, Zhao Q, Huang H, Yang B, Huang C. Association of Cardiac Injury With Mortality in Hospitalized Patients With COVID-19 in Wuhan, China. JAMA Cardiol. 2020 Jul 01;5(7):802-810.
- Maiese A, Frati P, Del Duca F, Santoro P, Manetti AC, La Russa R, Di Paolo M, Turillazzi E, Fineschi V. Myocardial Pathology in COVID-19-Associated Cardiac Injury: A Systematic Review. Diagnostics (Basel). 2021 Sep 08;11(9).
- Puntmann VOCarerj MLWieters I, et al. Outcomes of Cardiovascular Magnetic Resonance Imaging in Patients Recently Recovered From Coronavirus Disease 2019 (COVID-19). JAMA Cardiol. 2020;5(11):1265–1273.
- Uyanik M, Gedikli O, Yildirim U. Energy Drink-Associated Cardiomyopathy after Excessive Consumption: A Case Report. J Tehran Heart Cent. 2021 Jul;16(3):119-122.
- Caturano A, Galiero R, Vetrano E, Sardu C, Rinaldi L, Russo V, Monda M, Marfella R, Sasso FC. Insulin-Heart Axis: Bridging Physiology to Insulin Resistance. Int J Mol Sci. 2024 Jul 31;25(15):8369.

Akanksha Sharma
Dr. Akanksha Sharma, Head Writer and creator of AtoZ of Pregnancy, is dedicated to empowering women, parents, and families through 360-degree knowledge. She and her team provide evidence-based advice to guide families through pregnancy, parenting and beyond.